Ultrasound imaging can monitor the exact drug dose and delivery site in the brain
Science Highlights
June 17, 2019
An ultrasound imaging technique called passive cavitation imaging was able to create an image and estimate the amount of a drug that crossed the blood-brain barrier to reach a specific location in the brain, according to a study by NIBIB-funded bioengineers at Washington University. The technique monitors the activity of microbubbles, microscopic bubbles that help create clearer ultrasound images using detectors to estimate the effects they have on the different biological structures – in this case, the brain.
The brain is responsible for a person’s most vital functions; therefore, the brain protects itself with a tough-to-penetrate boundary called the blood-brain barrier (BBB). However, there are times when disease treatments need to get beyond the BBB to treat an illness that has invaded the brain.
“Researchers are developing non-invasive approaches using microbubbles and focused ultrasound waves to disrupt the blood-brain barrier (FUS-BBBD) briefly,” explains Randy King, Ph.D., director of the program in ultrasound at the National Institute of Biomedical Imaging and Bioengineering (NIBIB). “As new techniques are established to permeate the BBB, we need complementary methods to monitor the delivery of treatments to ensure they are safely delivered to the site(s) of brain disease.”
Hong Chen, Ph.D., assistant professor of biomedical engineering and radiation oncology at Washington University in St. Louis, explained that FUS-BBBD is achieved by concentrating or focusing, sound waves emitted from a device called a transducer, to a specific location. Chen compared the concept to focused sunlight passing through a magnifying glass to a localized spot. In FUS, the ultrasound waves are concentrated with specially designed ultrasound generators and help focus the BBB opening at a specific brain location.
Microbubbles can be injected into the bloodstream to amplify the effects of the ultrasound waves on the blood vessels, thereby opening the BBB in a localized spot. Researchers can store drugs for treatments inside the microbubbles. The pressure generated by ultrasound pulses can cause the microbubbles in the bloodstream to expand, contract, and eventually burst. When the microbubbles break in BBB blood vessels, the pressure created gently massages the blood vessels and makes them permeable to drugs injected into the bloodstream or carried by the microbubbles.
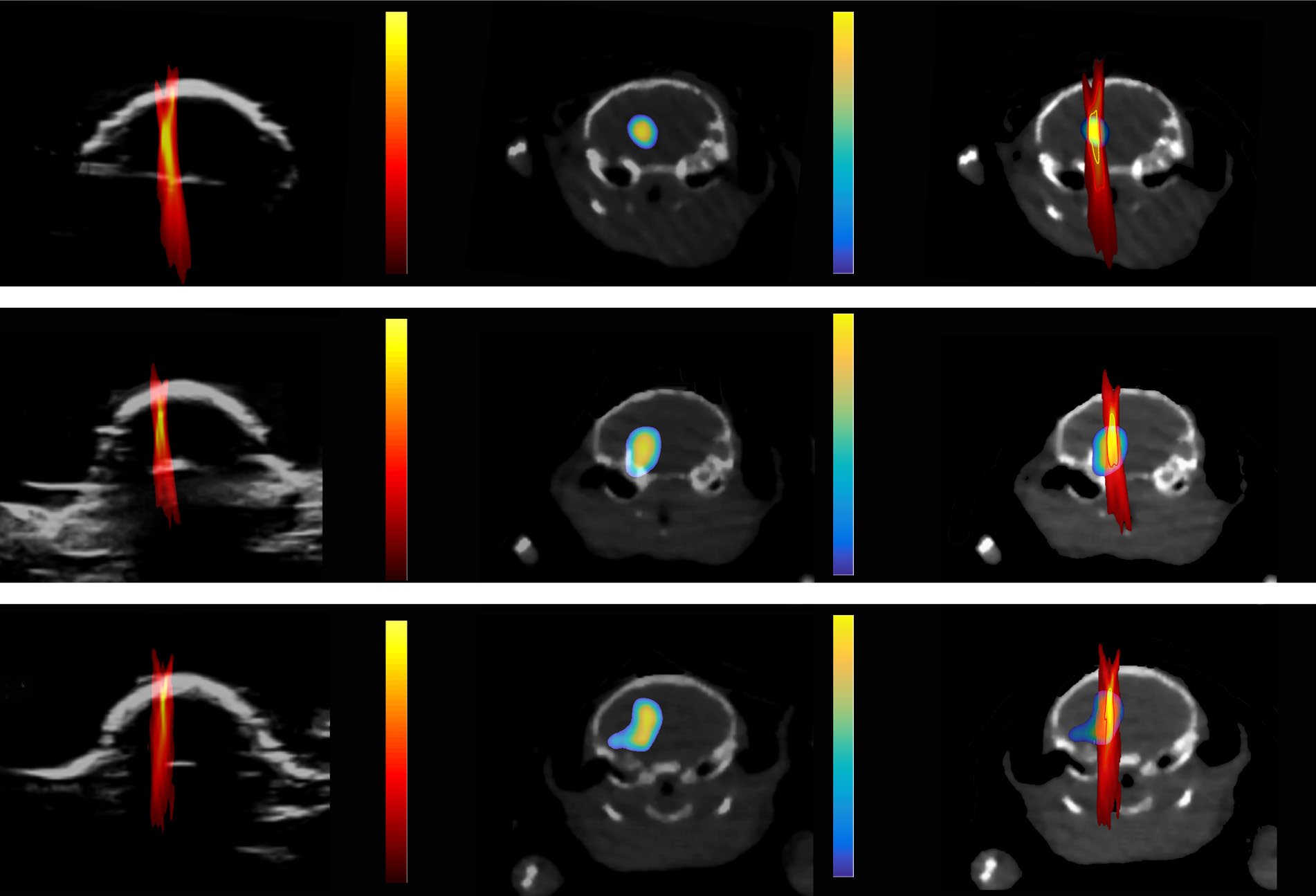
To track the amount and location of the drug delivered by FUS-BBBD, scientists labeled nanoparticles with a radioactive tracer and injected them into the blood circulation following FUS treatment. Then, positron emission tomography (PET) and computed tomography (CT) imaging were employed to measure and visualize the precise amount and location of the nanoparticles in the brain, respectively.
“The caveats to using PET/CT imaging are the associated exposure to radioactivity and higher costs,” explained Chen. The team wanted to find a cheaper, safer way to monitor where drugs go after they cross the BBB, so they explored a technique termed cavitation dose painting through passive cavitation imaging (PCI). The study was published in Scientific Reports.
Yaoheng Yang, the lead author of the study and a graduate student at Washington University, explained that PCI monitors the behavior of microbubbles in the ultrasound field and doesn’t rely on a radioactive particle like PET/CT imaging. Recording the dynamic behavior of the tiny bubbles allows researchers to create a detailed image that can track the location and amount of drug during FUS-BBBD treatment. But the question remained whether the PCI images would correlate to the PET/CT images.
“Our results demonstrated a pixel-by-pixel correlation between the PET and PCI images,” Chen stated. Chen is hopeful this advance in imaging will push the drug delivery field forward to better precision medicine. The team is calling the new technique cavitation dose painting because it is like “painting by numbers” for drug delivery.
With Chen’s new $1.6 million grant from NIBIB, she plans on fully integrating PCI with FUS-BBBD, so a doctor has full control over drug delivery. “With our new technique, we can predict exactly where a drug will go and how much of it will be released when it gets there. It helps us to minimize a drug harming healthy parts of the brain and avoid ineffective treatments when not enough drug reaches the intended target,” Chen declared.
This work was in part supported by the Children’s Discovery Institute of Washington University and St. Louis Children’s Hospital (grant number MC-II-2017-661), American Cancer Society (grant number IRG-15-170-58), and the National Institutes of Health (NIH) grant R01MH116981 and R01EB027223.
Yaoheng Yang et al, Cavitation dose painting for focused ultrasound-induced blood-brain barrier disruption, Scientific Reports (2019).